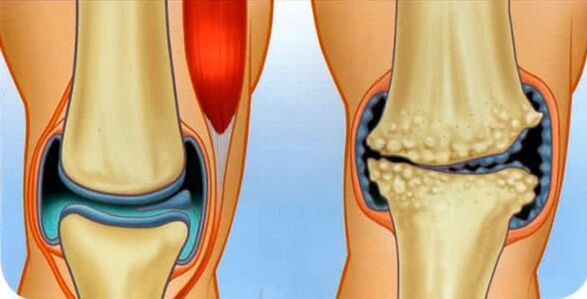
The surfaces of the bones that make up the joint are covered with a special, hyaline cartilage - smooth, articular surfaces that provide the least amount of friction during motor skills. If osteoarthritis is diagnosed, it means that the cartilage is in the process of being destroyed.
As it progresses, the destructive process spreads to the bones and then to the joint capsule.
The disease has a universal code for microbes 10 - M15-M19, classifying it as a class of pathologies of the musculoskeletal and connective tissues.
According to medical statistics, 12% of the world's population suffers from osteoarthritis, most of whom are elderly, over 65 years old. However, there is a worrying trend of increasing incidence among young people each year.
The diagnosis is not fatal, but it is insidious with the recurrence of osteoarthritis and the risk of complete disability.
Origin mechanism
The disease develops gradually, we can conventionally distinguish four stages:
- Initially, a cartilage area that is poorly supplied with blood or damaged is visible at the cartilage site. Gradually, in the presence of traumatic factors, the area does not recover, but rather grows.
- The body, trying to repair the broken cartilage, replaces the damaged areas with a mineralized tissue that does not have a clear structure. Such tissue is generally a low substitute for smooth, slippery and elastic hyaline cartilage.
- Gradually, the cartilage surface is covered with scars and bone growths - osteophytes.
- Healthy areas wear out very quickly from several times the load, and as a result, all the cartilage tissue becomes a large scar.
If the pathological process is not stopped, the joint will undergo the following negative changes:
- participates in the process of bone destruction;
- the synovial membrane becomes inflamed;
- the joint capsule loses its elasticity and tightens;
- the lumen of the joint cavity decreases rapidly;
- bones that cannot withstand friction are deformed as a whole as a joint;
- the tissues of the joint are reborn, thereby completely losing the ability to move.
Types of osteoarthritis
This disease affects absolutely any articular surface! At the same time, despite the same pathological mechanism, they are classified into several types.
Thus, they differentiate which joints are diseased:
- osteoarthritis of the knee joint or patellofemoral arthrosis (abbreviated as gonarthrosis);
- osteoarthritis of the hip joint (shortened coxarthrosis);
- arthrosis of the shoulder joint;
- interphalangeal arthrosis;
- arthrosis of the ankle joint;
- osteoarthritis of the hands;
- cervical arthrosis;
- jaw arthrosis;
- arthrosis of the metatarsophalangeal joint;
- arthrosis of the ilium;
- clavicular-acromial arthrosis;
- temporal arthrosis;
- osteoarthritis of the heels;
- arch arthrosis affecting the curved processes of the vertebrae (shortened spondyloarthritis);
- arthrosis of the facet articulation of the vertebral joints;
- uncovertebral arthrosis;
- costovertebral arthrosis;
- talonavicular arthrosis.
According to the characteristics of the pathological process in cartilage tissue, they are:
- deforming osteoarthritis is the name of a disease that has reached the terminal (final) stage;
- osteoarthritis - is characterized by the presence of a classic inflammatory process;
- chronic;
- acute osteoarthritis.
The causes of pathology are:
- dystrophic arthrosis of the joints associated with critical metabolic disorders;
- fractured arthrosis as a result of related injuries;
- post-traumatic osteoarthritis.
It is important to know! There is no arthrosis of the internal organs, for example, arthrosis of the heart is not a type of disease, but a consequence: a violation of heart function due to the destruction of cartilage in the chest.
There is another classification according to whether the disease is independent or caused by provocative factors:
- primary - occurs in completely healthy cartilage, another name - appears with idiopathic osteoarthritis or age-related changes in age;
- secondary - arises for many reasons.
Symptoms of osteoarthritis
There are very typical symptoms of osteoarthritis of all localizations, which differ in severity depending on the degree of development of the pathology:
- aggravated by aches, pain syndrome, high humidity and hypothermia;
- reduction of joint mobility;
- cracks, crackles and scratches during the movement of articular surfaces;
- external changes in the contour of the joint;
- swelling and edema;
- redness of the skin.
pain
The earliest signs of the disorder are mild to moderate, short-term pain that almost never occurs at night, but usually occurs only with a load on the articular surface.
When the inflammatory process reaches its final stage, the patient begins to feel unbearable, "taking" pain due to blood stasis and increased pressure in the joint sac. The pain is characterized by a long duration at any time of the day and regardless of whether the affected area is at rest or in motion.
joint stiffness
This symptom is characteristic of a fairly advanced disease. At the same time, in the early stages, the patient still feels discomfort when moving in the morning, after waking up, in the form of some stiffness.
With the development of destructive reactions, the patient notes:
- limiting the amplitude of ordinary movements;
- inability to change the position of the limbs at rest, even when trying to open the joint by hand;
- strong fixation (contracture) of the joint in a certain position in the absence of motor activity for a long time.
Finally, in the fourth stage of the pathology, ankylosis is formed in the form of scarring of articular tissues with complete loss of function.
Joint sounds
A crisis can be accompanied not only by osteoarthritis, but also any dysfunction of bones and cartilage.
However, the sound that is characteristic of this disease is:
- occurs only in painful joints;
- accompanied by difficulty in movement;
- tends to intensify with the development of pathology and enters during the formation of ankylosis.
Changing the appearance of the joint
Significant changes are visible in the later stages. Thus, the axis of the affected joint bends and the articular region itself is deformed - it grows in size, changes shape ugly.
All of this indicates the irreversible destruction of the joint, in which a new, non-specific tissue is formed.
If such a disease-causing process occurs in the knee, then the load on the ankle and metatarsophalangeal joints will increase, which over time will damage them.
If the externally deformed part of the body is also swollen or inflamed, it means that the synovial membrane is inflamed, so synovial fluid accumulates in large amounts in the joint sac and causes severe pain.
Causes of osteoarthritis
The pathology can occur in a single joint and can spread to several places. The disease occurs at a very young age - the body still has enough vitality to heal itself.
However, for all age groups, the reasons for their exposure are:
- internal - some diseases, bad habits, unbalanced diet, etc. ;
- external, - injuries, professional factor.
Internal causes are the factors that cause negative changes in the joint in the form of inflammation of the joint. There are inflammations of various origins:
- infectious (E. coli and Koch bacillus, viruses, chlamydia, staphylococci, Treponema pallidum, etc. );
- rheumatism;
- purulent arthritis;
- autoimmune nature;
- gout;
- psoriasis
In addition, causes of internal exposure include congenital or acquired disorders of cartilage structure and malnutrition, which may be related to:
- genetic failures and mutations;
- anomalies of intrauterine development, including perinatal trauma;
- forward age;
- osteoporosis, ie. "washing" of constituent elements from bone tissue;
- hormonal disorders and overload, including menopause;
- violation of normal metabolism;
- nutritional deficiencies of vitamins and minerals;
- diseases that cause muscle weakness;
- internal long-term intoxication.
Exacerbation of many diseases of the musculoskeletal system also causes cartilage degeneration.
External causes of the disease are factors that damage the joints, for example:
- frequent hypothermia;
- dislocations;
- strong blows;
- fractures;
- damage to the meniscus;
- strenuous physical activity (eg, lifting weights);
- professional sports;
- joint operation.
Degrees of osteoarthritis
There are four stages of osteoarthritis depending on the clinical manifestations and the progression of the disease:
- Grade 1 osteoarthritis is the initial stage of osteoarthritis characterized by latent symptoms in the form of adverse changes in the composition of synovial fluid and weakening of muscle fibers, if pain is seen, it is only during physical exertion;
- Grade 2 osteoarthritis - this is a feeling of pain due to the collapse of excess bones and the formation of osteophytes, the reflex neurotrophic regulation is impaired and a vocal murmur appears;
- Grade 3 osteoarthritis is characterized by significant degenerative changes in the joint, visible deformation with the curvature of the axis of the joint, shortening of the ligaments and pathological joint mobility of the joint;
- Grade 4 osteoarthritis is complete ankylosis, complete contracture, and even severe pain at rest.
All four stages continue unevenly: acute exacerbations and moments of remission are possible in the pathological period.
Treatment of osteoarthritis
It has been clinically proven that treatment and prevention in the form of removal of the triggers of hyaline cartilage damage, although it does not eliminate the disease at an early stage, stops its development and restores joint function.
In general, small and moderate diseases are treated conservatively. Surgical arthroplasty is indicated in case of severe destruction of the cartilage surface, which causes the destruction of bones.
The main principles of treatment in this case are:
- an integrated approach involving the use of several therapeutic methods;
- purposefulness, ie concentration of efforts to eliminate the factors and consequences of the disease.
Treatment with folk remedies
With a comprehensive treatment, but at home, you can additionally resort to therapeutic recipes of traditional healers who offer effective treatment of health problems through herbs and bee products.
Use of plants:
- Bay leaves in the form of decoctions, vodka tinctures and specially prepared oils are used directly on the area of inflammation;
- Honey treatment of osteoarthritis has proven to be a reliable topical remedy that eliminates inflammation in the form of friction and nourishes the skin, muscles and cartilage;
- cabbage leaf, - better than white cabbage, - knead a little and wrap it in a sore spot, heat it with a woolen cloth, and keep it all night;
- aloe juice in the form of compresses and rubbing into the skin;
Treatment of arthrosis of the knee joint with burdock also helps: the leaf is tied with a bandage to the painful area, which is isolated all night.
It is important to know! Using phytotherapy, you need to increase its effectiveness, forget about bad habits and pay attention to proper nutrition.
Medications for osteoarthritis
Drug treatment associated with the classical method of therapy is divided into drugs depending on the dosage form used:
- in the form of ointments for external use, arthrosis, abrasions, lotions;
- injections;
- pills for osteoarthritis;
- capsules.
Ointments
The pharmaceutical industry produces medical ointments based on natural, highly active ingredients:
- heparin ointment.
A remedy containing 1% diclofenac helps well: the gel is applied to the skin.
Injections
Injections have proven very good in treatment, not only intravenously and intramuscularly, but also directly to the affected area, for example, with non-steroidal drugs.
Thus, intraarticular injections are given into damaged joint tissues:
- glucocorticoids that strengthen the nutrition of cartilage tissue, eliminate inflammation and increase elasticity;
- chondroprotectors and analogues of intraarticular fluid;
- hyaluronic acid as a lubricant and analgesic.
Preparations in the form of tablets and capsules
A special group in drug therapy is called chondroprotectors for osteoarthritis, which contain structural elements of hyaline cartilage and thus restore it.
These drugs are available in the form of tablets and capsules intended for oral administration from the gastrointestinal tract (orally).
In addition, patients are prescribed NSAIDs - non-steroidal anti-inflammatory drugs for osteoarthritis, drugs that stop acute pain and eliminate inflammation.
Analgesics are also used in the form of novocaine blockade.
In addition, complex vitamins are prescribed for osteoarthritis.
Medicinal bile is recommended as a compress applied to the skin from topical natural preparations.
Exercises for osteoarthritis
Special exercises and therapeutic gymnastics (Therapeutic Gymnastics) have proven to be perfect, the complex provides gentle, dosed physical activity to the unhealthy part of the body.
Dr. Bubnovsky and Evdokimenko have developed their own set of therapeutic exercises.
It is important to know! Exercise is very effective in restoring health, but only if you apply it at the very beginning of the disease!
Massage for osteoarthritis
Therapeutic and medical massage, which improves the microcirculation and nutrition of deep tissues, has a very beneficial effect.
Diet for arthritis
In this case, it is important to follow a proper, rational diet to slightly improve the patient's condition. It is recommended to avoid overeating, animal fats and fried foods.
It is important to know! In addition, physiotherapy in the form of magnetic therapy, electrophoresis, paraffin and therapeutic mud dressings should be used in the fight for healthy cartilage.
Which doctor treats arthritis
First of all, you should go to a therapist with complaints of pain in the joints of the bones. He summarizes the patient's history and asks him in detail, referring to the necessary narrow specialist.
Depending on the cause of the disease and its type, there may be doctors with the following profile:
- orthopedist;
- traumatologist;
- surgeon;
- rheumatologist.


















